|
Eye
pain (may be severe) | |
|
Blurred or decreased vision | |
|
Sensitivity to light (photophobia) | |
|
Red eye | |
|
Tears | |
|
Smaller pupil on affected eye (sometimes) |

Red right eye in iritis
Your eye doctor may have diagnosed that you have a condition known as iritis. This is a condition where a part of the eye, the iris, becomes inflamed. With proper treatment an attack of iritis can be controlled.
|

Red right eye in iritis |
It
is more common for just one eye to be affected during an attack of iritis.
However both eyes can be affected at the same time.
Generally, the eye is not sticky, crusty or producing a discharge. These are symptoms more suggestive of conjunctivitis.
| The iris is the structure behind the cornea of
the eye which dilates and constricts. In bright light, the iris
constricts (you may have noticed this yourself). In dim light, it
dilates.
Image created by Mark
Erickson, CRA, COT |
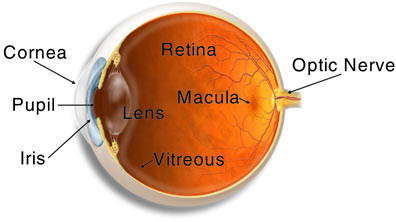 |
| The pupil is defined as the the hole in the middle of the iris. The
iris is the structure which is around the hole and defines the hole.
Image from American Academny of Ophthalmology |
 |
Yes.
Iritis is the commonest of a family of conditions called uveitis. The uvea
extends from the front of the eye to the back of the eye. Where the uvea is
inflamed at the front of the eye involving the iris,
uveitis is synonymous with iritis.
Where it inflamed near the middle of the eye involving the ciliary
body, it is called cyclitis. When
the back of the eye involving the choroid
is inflamed, it is called choroiditis.
|
Unknown
(this is the most common) | |
|
Certain
medical conditions such as: |
|
Injury
to the eye | |
|
Surgery
to the eye | |
|
Infections
such as: |
Parasite,
eg toxoplasmosis
Very
few people with iritis have a contagious variety. If you do, your doctor will
tell you.
Generally
speaking, no. No-one knows why people have recurrent attacks at particular
times. There is published evidence that earthquake victims have much higher
rates of recurrence so some doctors think stress may be a factor.
When
symptoms occur, a prompt examination by an ophthalmologist (medical doctor
specializing in the eye) is important. If left untreated, inflammation in the
eye can lead to permanent damage or even in extreme cases blindness.
The
ophthalmologist will use instruments to examine the inside of the eye and can
usually make the diagnosis on that basis. Since uveitis can be associated with
disease elsewhere in the body, he will require a thorough understanding of your
overall health. This may involve consultation with other medical specialists. He
may also request blood tests, X-rays, and other specialized tests to establish a
cause of the uveitis.
Eye
drops, especially steroids (such as Prednisolone
[PredForte]or Dexamethasone
[Maxidex]) and pupil
dilators, are medications used to reduce inflammation and pain in the front of
the eye. The steroid drops may need to be instilled frequently (in severe cases
as much as every half an hour). Your ophthalmologist will arrange to see you
again to assess the progress of the treatment and will, according to the degree
of inflammation, decrease or increase the treatment.
Pupil
dilating drops (such as Cyclopentolate
[Mydrilate] or Atropine) make you feel more
comfortable and prevent certain complications of iritis. However you may become
more sensitive to bright light, especially during the summer, and you may lose
the ability to focus on near objects (accommodation),
and your vision may become more blurred.
Steroids
taken by mouth have side-effects. However steroid eye drops are absorbed
principally by the eye and do not cause the same side-effects as oral steroids.
In a small proportion of people steroid eye drops cause the pressure in the eye
to rise above normal. Your ophthalmologist will measure the pressure in the eye
to discover if you are one of these people and will treat you accordingly.
In
most cases complications are rare, but they include:
|
Glaucoma
(high pressure in the eye causing damage) | |
|
Cataract
(clouding of the lens of the eye) | |
|
New
blood vessel formation (neovascularization) |
These
complications may themselves need treatment. If complications are advanced,
conventional or laser surgery may be required.
Uveitis
arising in the front or middle of the eye (iritis
or cyclitis) is commonly more sudden
in onset, generally lasting six to eight weeks, and in early stages can usually
be controlled by the frequent use of drops. Often, this type of uveitis cannot
be given a specific cause.
Uveitis
in the back part of the eye (choroiditis)
is commonly slower in onset and may last longer, and is often more difficult to
treat. Treatment may involve steroid tablets or injections. Often, multiple
tests are required to find the cause of this type of uveitis.
With
infections, uveitis tends to clear up once the underlying infection is treated.
You
should not drive a car if you canít see properly. Dark glasses will make you
feel more comfortable. Whether you will need to give up work depends on the
severity of the symptoms. There is no special diet required.